Airway Epithelial Cell Contribution to Immune Responses to Pulmonary Fungal Pathogens
In the human host, the airway epithelium is the first point of contact upon inhalation of fungal conidia. As an immunologically active tissue, the airway epithelium may participate in active phagocytosis and coordinated immune cell recruitment. We have two primary projects centered on the impact of respiratory epithelium in infections: [1] coccidioidomycosis and the airway epithelium, and [2] airway epithelial-mediated immune responses to pulmonary fungi.
Coccidioidomycosis and the Airway Epithelium
Soil fungi, including Coccidioides, do not need a human host to propagate, but upon disruption can enter the human body and lead to infection if not cleared. The fungal dimorph Coccidioides is native to arid regions in the southwestern US and can establish infections in both immunocompetent and immunocompromised individuals. Unfortunately, little is known with regards to the initial response of human airway epithelium to Coccidioides. Our lab utilizes both the wildtype and an avirulent strain (Δcps1) developed in the Galgiani lab. The Δcps1 strain is a potential vaccine candidate. We are currently leveraging this strain compared to wildtype to dissect secretomal and transcriptional differences in the airway epithelium that mount a successful response to Coccidioides. This work was recently funded by the NIAID through an R21 mechanism.
Coccidioides arthroconidia (left) and spherule (right).
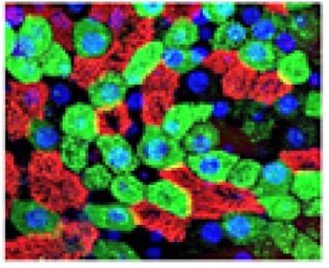
Airway Epithelial-Mediated Immune Response to Pulmonary Fungi
Recent advances enable us to isolate airway basal cells from patients to be expanded into fully differentiated airway epithelium. Similarly, murine airway basal cells can be expanded into the airway epithelium. Utilizing an air-liquid interface (ALI) system, we can examine apical and basolateral responses of airway epithelium as well as the recruitment of critical immune cells to pathogens. This model enables the dissection of cellular pathways at play in primary human samples. Additionally, this system provides the opportunity to probe intrinsic differences in patients at high risk of infection. In addition to this in vitro model, we use in vivo pulmonary infection genetic models in to investigate the role of respiratory epithelium in mediating antifungal immunity. This project focuses on two pulmonary fungi: Aspergillus and Coccidioides. We hope to provide a window into the coordinating role of airway epithelium in innate immune and identify new therapeutic strategies for pulmonary fungal infections.

